Transoral incisionless fundoplication (TIF) is an advanced endoscopy procedure which mimics surgery but in a minimally invasive way. It is performed via endoscope and takes less than 30 minutes.
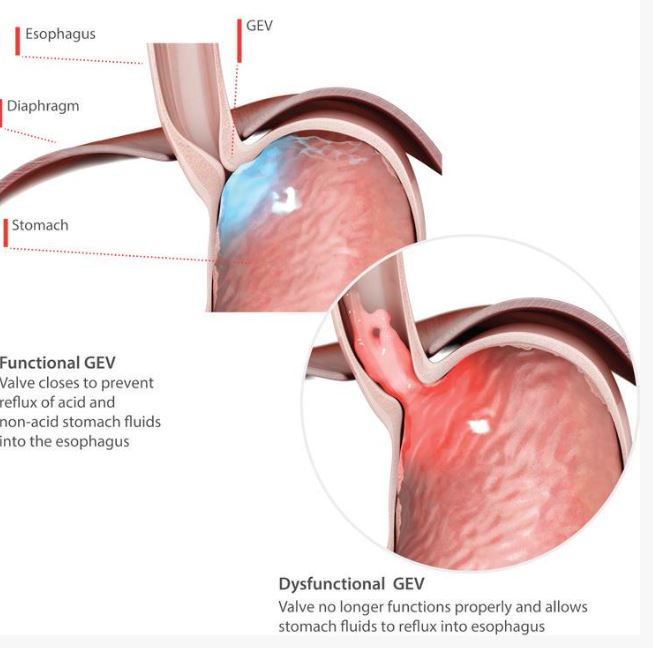
The bottom of the food pipe is pushed into the stomach and stitched into place creating a new ‘anti reflux valve’ for the patient that prevents stomach contents leaking up. Unlike anti-reflex surgery the patient can still burp/vomit which many patients find reassuring.
TIF recovery is quick – most people are back home within 1 day and back at work within 4 days and it’s very safe, less than 0.5% patients will experience a serious problem.
Studies have shown that for up to five years after the TIF procedure, GORD symptoms are significantly reduced and around 80% of patients can stop taking daily heartburn drugs. In a recent study published from Johns Hopkins hospital in the USA, 49 patients with LPR and evidence of GORD had the TIF procedure and experienced an improvement in their symptoms.
The TIF procedure reduces the chronic acid reflux and reduces the harm to the cell lining (which may have turned cancerous over time).
TIF
- TIF mimics what surgeons do, but it’s completely incisionless (performed via endoscopy)
- TIF takes around 30 minutes and doesn’t require surgery
- TIF patients maintain normal functions such as the ability to belch and vomit
- There is very little risk of swallowing problems (1%) after the TIF procedure
SURGERY
- Surgery involves multiple incisions in the patient’s abdomen
- Surgery takes significantly longer
- Patients lose the ability to vomit, which some patients find distressing, and burping/belching function can be limited.
- Surgery typically includes side effects such as difficulty swallowing (10-15%), bloating, and increased flatulence
- Surgery is the best option for those with large hiatal hernias
In a recent study of hiatal hernia repair with TIF vs Nissen Fundoplication (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9812651) the following was noted:
Results A total of 125 patients with HH repair with TIF and 70 with HH repair with LNF were compared. There was no difference in rates of discontinuing or decreasing proton pump inhibitor use, dysphagia, esophagitis, disrupted wrap, and HH recurrence between the two groups ( P > 0.05). The length of hospital stay (1 day vs. 2 days), 30-day readmission rate (0 vs. 4.3 %), early AE rate (0 vs. 18.6 %), and early serious AE rate (0 vs. 4.3 %) favored TIF (all P < 0.05). The rate of new or worse than baseline bloating was lower in the TIF group at 6 months (13.8 % vs. 30.0 %, P = 0.009).
Conclusions Concomitant HH repair with TIF is feasible and associated with lower early and serious AEs compared to LNF.